Key Takeaways:
- Specialized Expertise: Neurologists focus on a wide range of conditions, including stroke, epilepsy, movement disorders, and neurodegenerative diseases, each demanding clinical precision, curiosity, and compassionate care.
- Complex Case Management: Common neurological conditions like Alzheimer’s, Parkinson’s, multiple sclerosis, and epilepsy challenge neurologists to combine deep scientific understanding with human empathy.
- Extensive Training Journey: Becoming a neurologist requires years of education and hands-on training, but the path is grounded in purpose—unraveling the complexities of the brain to improve patient lives.
When people think of neurologists, they often picture specialists treating seizures or memory loss—but the field is far more expansive. Neurologist specialties span a broad spectrum of brain, spine, and nerve conditions, from managing movement disorders to investigating chronic headaches. Each subspecialty brings unique challenges, requiring physicians to combine diagnostic precision with long-term patient care.
For medical students exploring their options, gaining clarity on these specialties is essential. That’s why OnlineMedEd is here to break down complex topics into approachable, high-yield learning—so you can connect classroom knowledge with real-world care. In this article, we’ll walk through the major fields within neurology, what each subspecialist does, and how they help patients navigate some of the most complex conditions in medicine.
Understanding The Role Of Neurologists
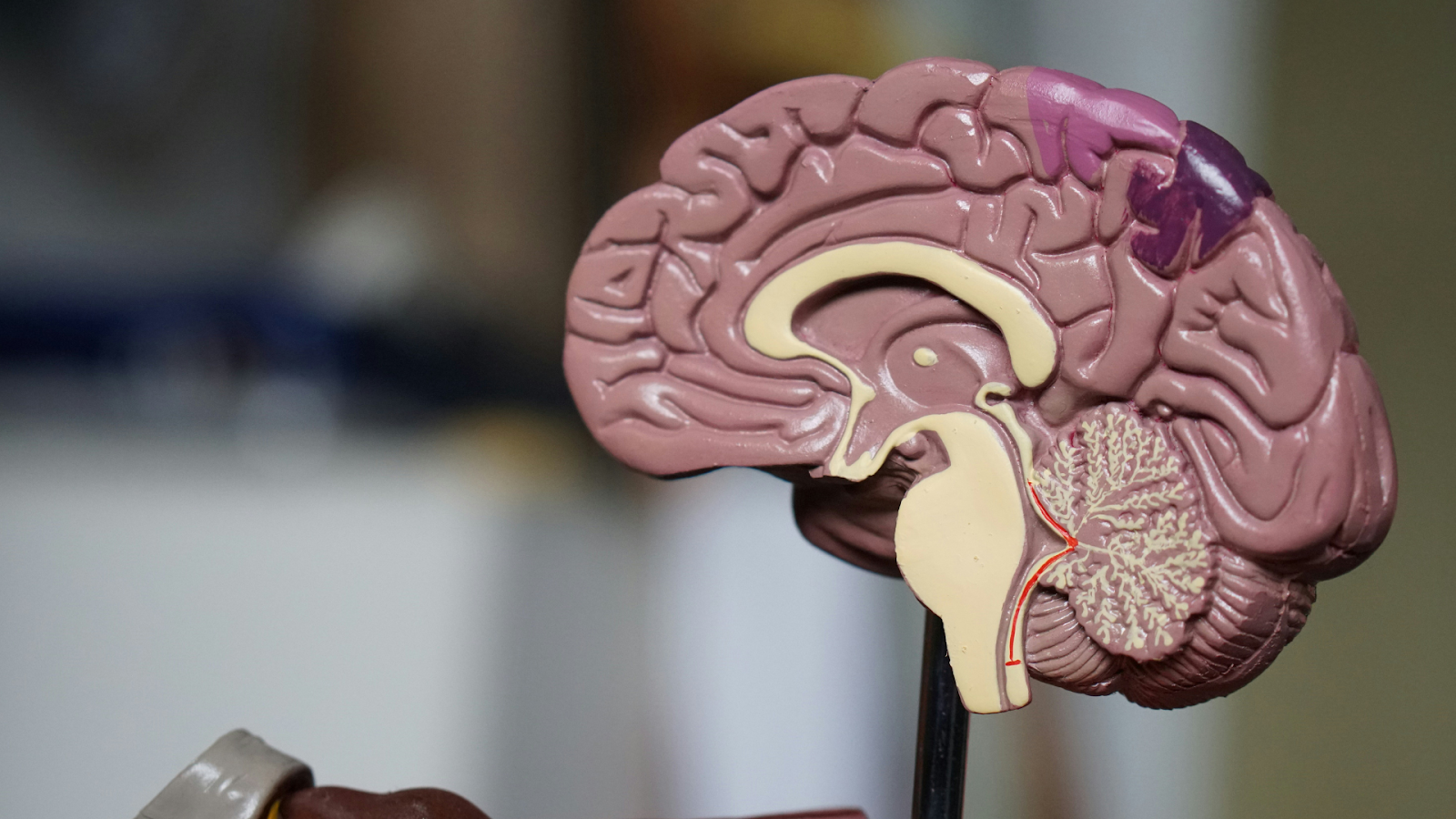
Let’s get to the heart of what neurologists do. These aren’t just doctors who test reflexes and move on. Neurologists are the investigators of the nervous system, diving into the complexities of the brain, spinal cord, and peripheral nerves to diagnose and manage a wide array of disorders. They handle cases that range from chronic migraines and movement disorders to acute emergencies like strokes, often managing conditions that evolve slowly over time or appear without clear cause.
Their diagnostic approach is methodical and nuanced. Neurologists gather evidence to answer difficult clinical questions using tools like MRI, CT, EEG, and lumbar puncture. But tests only go so far. Interpreting them requires clinical reasoning, pattern recognition, and the ability to synthesize symptoms into a coherent diagnosis. In many ways, neurologists are the clinical detectives of medicine, relying on deep knowledge and experience to solve complex patient puzzles.
Neurology In Action: Balancing Science And Humanity
Consider the patient whose memory is fading, or the young adult with sudden tremors. A neurologist doesn’t stop at symptom management. They construct a diagnostic narrative that guides testing, treatment, and long-term planning. Sometimes this means identifying treatable conditions like multiple sclerosis or epilepsy. Other times, it involves navigating the emotional terrain of progressive diseases like Parkinson’s or ALS, where the focus shifts to improving quality of life and supporting both patient and family.
Compassionate communication is key. Neurologists often face the difficult task of delivering life-altering diagnoses. But in doing so, they also offer clarity, stability, and next steps—whether through medications, therapy, referrals to subspecialists, or coordinated care planning.
Small Victories In A Complex Field
Despite the challenges, neurology isn’t all crisis and decline. Neurologists are also part of remarkable success stories: a patient walking again after spinal cord trauma, or a child with epilepsy gaining seizure control through treatment. These moments are grounded in evidence-based practice, collaborative care, and the neurologist’s unwavering commitment to their patients' well-being.
Neurology is not a specialty you master through studying alone; it’s one you grow into. OnlineMedEd’s clinically driven learning tools for future providers can support that growth. By reinforcing concepts through whiteboard lectures, challenge questions, and integrated notes, you can build the diagnostic instincts that neurology demands, one case at a time.
The Journey To Becoming A Neurologist
Every neurologist’s path begins with a four-year undergraduate degree, typically in a science-focused major like biology, neuroscience, or chemistry. Students must complete pre-med requirements while gaining clinical exposure through shadowing and volunteering. The goal isn’t just academic success; it’s preparation for the rigors of medical school and the realities of patient care. Success also hinges on performance on the Medical College Admission Test, a mandatory entrance exam that assesses your critical thinking, scientific problem-solving skills, and social and natural science knowledge.
Medical School: Preclinical And Clinical Training
Once accepted into medical school, students enter a four-year program that blends foundational science with hands-on learning.
- Preclinical Phase: The first two years are lecture- and lab-heavy, covering subjects like neuroanatomy, pharmacology, and pathology. OnlineMedEd’s Preclinical curriculum helps learners solidify these fundamentals in a clinically relevant way, ensuring they retain this information for life.
- Clinical Phase: The final two years are focused on clinical rotations, where students rotate through neurology, internal medicine, psychiatry, and other specialties. During this phase, you’ll begin to apply core knowledge in real-world settings—seeing stroke presentations, seizure management, and neurodegenerative conditions firsthand. Here, OnlineMedEd’s Clinical content can help you personalize and maximize your learning with integrated notes, whiteboard video lectures, multiple-choice challenge questions, and memory-enforcing activities. Not only will you impress on rounds, but we can also help you build a strong foundation for success on shelf and licensing exams.
To advance, students must also pass the USMLE Step 1 and Step 2 CK exams. OnlineMedEd’s USMLE test prep helps reinforce retention and clinical reasoning through concept-based learning and spaced repetition. You’ll be prepared to excel no matter what curveballs these exams throw your way.
Neurology Residency: Specialized Training
After medical school, neurologists match into a four-year neurology residency—typically beginning with a one-year preliminary internal medicine internship, followed by three years of neurology-specific training. During residency, trainees typically manage patients with stroke, epilepsy, multiple sclerosis, neuropathies, and more. You’ll also gain competency in procedures like lumbar punctures and EEG interpretation while collaborating across inpatient, outpatient, and ICU specialties. Most importantly, you’ll develop the communication skills necessary for delivering complex diagnoses with empathy.
Residency is demanding, but it’s also where neurologists develop the confidence and clarity to lead care for patients with some of medicine’s most complex conditions. For dedicated residents who are interested in maintaining clinical competency and expanding their professional skills, OnlineMedEd offers a suite of GME resources to help reinforce core knowledge while supporting long-term success and growth. You’ll be able to consistently review refreshers on clinical concepts while learning about the best practices and operational tools for doctors.
Licensure, Board Certification, and Continuing Education
Along the way, residents complete the final stages of USMLE or COMLEX testing and prepare for board certification by the American Board of Psychiatry and Neurology (ABPN). Even after training, the learning continues. Neurologists pursue continuing medical education (CME) to stay current on advances in neuroscience, imaging, therapeutics, and patient-centered care.
A Career That Demands And Delivers Purpose
The path to neurology isn’t short, and it’s not easy. But it's a path worth every step for those driven to decode the human brain, ease suffering, and deliver answers where there often are none. In this field, you’re preparing to listen deeply, think critically, and care for patients in some of their most vulnerable moments. It’s a specialty built on both science and soul—and it requires providers who are committed to both. With the right tools, mentorship, and a strong foundation, the medical education journey prepares future neurologists not just to treat disease but to change lives.
Neurologist Specialties: Exploring The Many Fields Of Brain And Nerve Care
Neurology is an incredibly expansive field. Once core training is complete, many neurologists pursue additional fellowship training to focus on a particular population, condition, or diagnostic approach. These subspecialties allow for even deeper expertise and more tailored care, because when it comes to the brain and nervous system, precision matters.
- Pediatric Neurology: Focuses on diagnosing and managing neurological conditions in infants, children, and adolescents, from seizures to developmental delays.
- Neuro-Oncology: Specializes in treating brain and spinal cord tumors, including care coordination across surgery, radiation, and chemotherapy.
- Neuromuscular Medicine: Addresses diseases affecting nerves, muscles, and the neuromuscular junction, like ALS, muscular dystrophy, and myasthenia gravis.
- Vascular Neurology: Dedicated to stroke prevention, acute treatment, and post-stroke care, including TIA evaluation and risk factor management.
- Neurocritical Care: Manages life-threatening neurologic conditions in the ICU setting, including traumatic brain injuries, status epilepticus, and severe strokes.
- Headache Medicine: Focuses on chronic and complex headache disorders, such as migraines, cluster headaches, and tension-type headaches.
- Sleep Neurology: Evaluates and treats neurologically rooted sleep disorders such as narcolepsy, REM behavior disorder, and sleep apnea.
- Neuroimmunology: Specializes in autoimmune conditions that affect the nervous system, including multiple sclerosis and neuromyelitis optica.
- Movement Disorders: Centers on conditions like Parkinson’s disease, essential tremor, dystonia, and Huntington’s disease.
- Clinical Neurophysiology: Uses tools like EEG, EMG, and nerve conduction studies to assess brain, spinal cord, and nerve function.
- Behavioral Neurology: Explores cognitive and emotional symptoms tied to brain conditions, including dementia, aphasia, and personality changes.
- Epilepsy Management: Focuses on seizure diagnosis and treatment, often incorporating advanced imaging, medication management, and surgical evaluations.
- Neurorehabilitation: Aims to restore function and improve quality of life after neurologic injury or illness through multidisciplinary therapy.
- Pain Medicine In Neurology: Addresses complex neurological pain syndromes such as trigeminal neuralgia or central pain after stroke.
Each of these subspecialties brings something critical to the table. Whether addressing urgent crises or long-term chronic conditions, they represent the depth and diversity of neurologic care—and the opportunity to make a meaningful difference at every stage of life and disease.
Final Thoughts
Neurology is one of medicine’s most challenging and meaningful fields, and breaking down its subspecialties reveals just how much precision, empathy, and resilience it demands. At OnlineMedEd, we’re committed to supporting students with a unified, learner-first approach that builds knowledge and lasting confidence. With tools like our PACE framework, whiteboard videos, and challenge questions, we help you truly learn—so you’re prepared to meet the complexities of brain and nerve care with clarity, compassion, and purpose.
Whether you’re a student grappling with the complexities of neurology or a faculty member striving to inspire, OnlineMedEd is your partner in redefining medical education. Let’s illuminate this path together, ensuring you learn for real and do good in the world.
Read also:
- Internal Medicine vs. Family Medicine
- Mentoring In Medicine
- Neurology Lifestyle: Work Hours, Salary, And Job Satisfaction
Frequently Asked Questions About Neurologist Specialties
What is a neurosurgeon, and how do they differ from neurologists?
Let’s clear up a common point of confusion. Neurosurgeons are medical doctors trained to perform surgical procedures on the brain, spinal cord, and peripheral nerves. They handle structural problems—think tumors, aneurysms, traumatic injuries, and herniated discs—where operating is necessary. Neurologists, on the other hand, are non-surgical specialists who diagnose and treat nervous system disorders like epilepsy, multiple sclerosis, or migraines through medications, lifestyle recommendations, and other therapies. Both play vital roles in brain and nerve care, but their approaches differ: one operates, the other manages.
What subspecialties exist within neurology?
Neurology is made up of diverse subspecialties that address everything from chronic migraines to life-threatening strokes. For example, vascular neurologists focus on stroke prevention and emergency treatment, while movement disorder specialists help patients manage conditions like Parkinson’s disease and essential tremor. Pediatric neurologists care for children with developmental or genetic brain conditions, and neurocritical care specialists oversee patients in the ICU with severe brain injuries.
Each subspecialty presents unique challenges and requires sharp clinical skills, deep empathy, and constant learning—skills we help build at OnlineMedEd through clinically integrated content. For a full overview of neurologist specialties, check out the complete list in the article above.
What are the qualifications of a neurointensivist?
A neurointensivist is a neurologist (or sometimes an anesthesiologist or neurosurgeon) who specializes in managing critically ill patients with severe brain or spinal cord injuries. After completing medical school and a neurology residency, they pursue a fellowship in neurocritical care, typically lasting one to two years. During this time, they develop advanced skills in managing acute stroke, brain hemorrhage, post-operative care, and multi-organ support in ICU settings. Board certification in neurocritical care may follow, validating their expertise. The training is intense, but necessary for a role that often means life or death decisions.
What role does a neurogeneticist play in patient care?
Neurogeneticists specialize in diagnosing and managing neurologic conditions with a genetic basis, like Huntington’s disease, muscular dystrophies, and some epilepsies. They utilize tools such as genetic testing and counseling to provide clarity for families facing inherited disorders. Beyond diagnosis, they guide long-term treatment plans, collaborate with researchers, and often engage in clinical trials to explore cutting-edge therapies. It’s a field that bridges science with human connection.
What are the latest advancements in neurology specialties?
The field of neurology is rapidly evolving. AI tools now assist in analyzing imaging for earlier detection of diseases like Alzheimer’s. In stroke care, extended thrombectomy windows and improved imaging have broadened treatment options. Neurogenetics is advancing with gene therapies and CRISPR-based techniques, which show promise for conditions once considered untreatable. Deep brain stimulation is becoming more precise for managing Parkinson’s and other movement disorders. Wearable devices also give patients real-time feedback on managing conditions like epilepsy or migraines. At OnlineMedEd, we constantly update our resources to reflect these innovations, helping learners stay current with what matters most.
How do neurologists perform diagnostic tests?
Neurologists rely on a wide array of diagnostic tools to pinpoint the root cause of a patient’s symptoms. A neurologic exam assesses reflexes, strength, coordination, and sensation. Imaging studies like CT or MRI help visualize brain and spinal structures. EEGs track brain wave activity, commonly used for epilepsy and sleep studies. EMG and nerve conduction studies evaluate muscle and nerve function in neuromuscular diseases. Lumbar punctures may be used to assess for infections, inflammation, or bleeding in the central nervous system. Understanding these tests—and when to use them—is core to the practice of neurology.