Though Africa’s first COVID-19 case appeared in Egypt on February 14, it didn’t really start making noise around the continent until the following month.
By mid-March, the World Health Organization (WHO) had declared a global ‘pandemic’ and Wall Street buckled as the extent of COVID-19’s reach revealed itself.
Italy, Spain and Iran suffered in the novel coronavirus’s shocking first wave, before, in New York City, the United States was dragged into the fold.
While COVID-19’s spread in Africa was initially slower than other regions, public health experts around the world worried about the potential havoc it could wreak among its 1.2 billion strong population.
Most African countries don’t have a peak. I don’t understand why. I’m completely at sea.
Similar to Brazil, high population density, inconsistent health care facilities, and a potential inability to contact trace a quickly spreading virus led some to warn ‘millions’ of Africans could die.
One prominent South African health official thought “we were heading towards a disaster, a complete meltdown.”
Yet despite ongoing outbreaks in South Africa, Libya, and a handful of other countries, Africa has—so far—dodged the worst of the global pandemic in a way that has left the experts scratching their heads.
Though the continent’s low median age, aggressive government pandemic responses road-tested by earlier disease outbreaks, and effective public health messaging have all been suggested as potential reasons for its lower death tolls—and potentially higher asymptomatic rate—measurable reasons for Africa’s relative success remain unclear.
“Most African countries don’t have a peak,” Professor Salim Karim, one of South Africa’s leading epidemiologists, told the BBC. “I don’t understand why. I’m completely at sea.”
Differences in experience
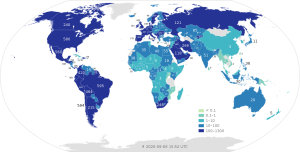
As of today, there have been 1,322,452 confirmed COVID-19 positives in Africa, with 31,913 dying from its complications (around the same as France). Close to half of all deaths, and positive cases, have come from South Africa.
With more than 191,000 dying from COVID-19, and more than 6.3 million testing positive, the U.S. is still in the midst of the pandemic’s brutal second wave that has seen Texas, Florida, Arizona, and Georgia particularly hard hit.

More people have died of COVID-19 in Georgia than Egypt, Africa’s second worst hit nation. If Mississippi and Alabama were African nations, they would have the third and fourth worst death tolls on the continent.
Unlike the U.S, Africa reacted quickly when the first reports of a coronavirus outbreak in China begun to circulate, in late 2019. As early as January 2, the Ivory Coast began beefing up surveillance at airports, with all passengers with recent travel to China received extra screening.
Quickly adopted by many other African nations, the aggressive measures came nearly two weeks before the first confirmed COVID-19 case outside China, in Thailand.
With virtually all flights later cancelled to China, an important trade partner across Africa, the continent’s COVID-19 numbers stayed minimal until travelers from Europe are thought to have bought the virus in, by early March.
By the end of the month, most African nations had enforced travel bans on deeply infected Asian and European countries, with quarantines made mandatory for all incoming travelers.
Africa has invested in preparedness and response efforts geared toward various outbreaks on the continent … this technical know-how has been swiftly adapted to COVID-19.
By the end of April, more than 40 African nations had closed their borders, while strict rules around movement and public gatherings were bought into place. Though often homemade, face masks became common.
Under the lead of the Africa Center for Disease Control and Prevention (Africa CDC) and WHO, COVID-19 testing labs went from 2 in February to 43 in mid-March. Rapid tests started being researched in Senegal around the same time.
By mid-May, 33 COVID-19 clinical trials were in operation in Africa, with capacity in place for ten more. South Africa has since been included in crucial global phase II vaccine trials now being conducted.
Road-tested responses, and dubious numbers
Experts say the continent’s earlier experience of disease outbreaks like Ebola, which claimed more than 11,000 lives in Guinea, Liberia, and Sierra Leone between 2014 and 2016, helped prepare it for COVID-19.
A pragmatic ‘do it yourself’ approach to the pandemic’s required health and economic mandates has also helped, as has little opposition to mask wearing.
“Africa has invested in preparedness and response efforts geared toward various outbreaks on the continent (such as Ebola virus disease, Lassa fever, polio, measles, tuberculosis and human immunodeficiency virus),” wrote six authors of an extensive article on Africa’s coronavirus response for Nature Medicine, in June.
“This technical know-how has been swiftly adapted to COVID-19. Continental exchange platforms with an established wide audience have been repurposed for training and information on COVID-19 diagnostics.
“Networks of community health agents that support the response to polio and other diseases have been leveraged for sensitization and to raise the alarm about the suspected COVID-19 at the subnational level.”
Though the continent-wide response was strong from the get-go, the WHO and International Rescue Committee have cautioned against using the data currently available when attempting to understand the true scale of the pandemic in Africa.
With half of the continent’s nations having a ratio lower than the Africa CDC recommended benchmark of 10 tests per positive case, it’s difficult to know how many million positive cases have slipped through the proverbial cracks.
The BBC used the differing testing strategies of Kenya and Ethiopia to illustrate the likely strength of the virus. Kenya now only tests high-risk groups for COVID-19, while Ethiopia aimed to ramp its capacity up to 400,000 a month.
While rates in Ethiopia have gone up, Kenya’s have dropped, as have most around the continent (where testing is far below where it needs to be). Perhaps as a result; WHO statistics have shown a 14 percent drop in positive COVID-19 cases since early August.
… many hospital beds remain empty, and where infection graphs have almost entirely avoided the pronounced peaks and sharp angles seen in so many other parts of the world.
Yet last month, Science reported that studies following a test of more than 300 Kenyan blood donors showed an estimated five percent of the country was likely to have SARS-CoV-2 antibodies, showing previous infection.
“That would put Kenya on a par with Spain in mid-May when that country was descending from its coronavirus peak and had 27,000 COVID-19 deaths,” Linda Nordling wrote, for Science.
Just over 600 Kenyans have died in the pandemic, while many of its hospitals are not reporting large numbers of patients with coronavirus symptoms.
It has been suggested that the relative youth of Africa has potentially contributed to the—likely—higher rates of infection, but lower death tolls (he median population age across the continent is 19.7, compared to 38.6 in the U.S).
However, studies have indicated that, based on global age-specific case fatality rates, COVID-19 deaths in Africa should only be four times less than those of Europe and North America, rather than the 20 they are today.
Struggling nations
Despite the relative public health success in Africa, the impact has been far from uniform.
Eleven African nations, out of 54, currently have COVID-19 death rates close to, or higher than, the global average of 3.3 per cent.
Uganda, Rwanda, Morocco and Tunisia are amongst those that have seen recent increases in positive rates. Libya, in particular, is in the midst of a brutal wave, with positive rates doubling over the last two weeks of August.
Now with 20,462 overall cases, Libya’s has recorded around 77 COVID-19 cases per 100,000 population over the last week, which is higher than the U.S. (76 per 100,000).
With only half of all hospitals and health facilities currently operating due to damage from recent domestic turmoil, their healthcare system is barely set up to deal with the ill.

Economically, the entire continent of Africa is on the ropes following the extreme early measures. The United Nations has warned of a “full-blown financial crisis,” with potential funding shortfalls for public health of serious concern.
After implementing one of the world’s strictest nationwide lockdowns in March, a fast-growing recession forced South Africa’s leaders to ‘re-open’ the country up over the last three months.
By late July, Reuters described South Africa as facing a “runaway epidemic” that strained its public health system and saw the nation achieve the eighth most COVID-19 cases in the world.
South Africa is emerging from its first wave of infection with a COVID-19 death rate roughly seven times lower than Britain’s.
Yet “… today,” Andrew Harding, the BBC’s head African correspondent wrote on September 2, “South Africa is emerging from its first wave of infection with a COVID-19 death rate roughly seven times lower than Britain’s.”
“Scientists acknowledge that reliable data is not always easy to come by and all these figures are likely to change,” Harding continued.
“But even if deaths have been under-reported here – perhaps by a factor of two – South Africa has still performed impressively well, as have many other parts of the continent, where many hospital beds remain empty, and where infection graphs have almost entirely avoided the pronounced peaks and sharp angles seen in so many other parts of the world.”
This could change, of course, but understanding how Africa was even able to arrive at this point will be crucial in our overall understanding of the COVID-19 global pandemic.



